Hormone Imbalance and Sleep Disorders: Restoring Restful Sleep
Restful sleep is crucial for your health and well-being. More than just maintaining our energy levels, sleep regulates our hormones, which control everything from mood and metabolism to reproductive health. Still, it can be challenging to prioritize a good night’s rest in our fast-paced world. In fact, up to 35% of adults experience insomnia symptoms, while 42% of women in their perimenopause ages experience hormonal insomnia.
Hormone balance may help support more restful sleep. Read on to explore the relationship between sleep and hormonal health, and how to reclaim your sleep.
Understanding the Sleep-Hormone Connection
Hormonal health is closely associated with our sleep cycle. For example, hormonal changes that happen in pregnancy and menopause can lead to sleep disorders. Additionally, the stress hormone cortisol is associated with sleep problems, underscoring their complex relationship.
Human sleep cycles involve different stages, including light sleep, deep sleep and rapid eye movement (REM) sleep. These stages are essential for producing and regulating different types of hormones. Disruptions in the sleep cycle can prevent the body from reaching these stages, which can, in turn, impact hormone levels.
Furthermore, our circadian rhythm, the body’s internal clock, regulates the release of cortisol and melatonin in sync with the day-night cycle. Disrupting the circadian rhythm by staying up late or working night shifts can, therefore, lead to hormonal imbalances.
Key Hormones That Affect Sleep
Hormones that affect sleep include:
- Melatonin: Produced by the pineal gland, melatonin levels rise in the evening in response to darkness, signaling the brain that it’s time for sleep. Our body’s internal clock regulates melatonin production, but it naturally declines with age, which is why many older adults experience sleep disturbances and insomnia. Supporting healthy melatonin production and overall hormone balance may help improve sleep quality, especially with age.
- Cortisol: Cortisol plays a big role in our sleep cycle pattern. It is higher in the morning to promote alertness and lowest at night before we go to bed. However, prolonged stress elevates cortisol levels and disrupts their natural rhythm. At night, higher cortisol levels can suppress melatonin and increase alertness, leading to insomnia.
- Thyroid hormones: The thyroid gland produces hormones — T3 and T4 — that control metabolism and energy use. People with hyperthyroidism, or an overactive thyroid, can have more anxiety, a racing heart and insomnia. In contrast, an underactive thyroid can lead to fatigue, snoring, daytime sleepiness or sleep apnea risk.
- Estrogen: Estrogen is mainly known for regulating the menstrual cycle. It also affects body temperature and serotonin production, both of which areimportant for mood and sleep. During perimenopause and menopause, estrogen levels can decline and cause hot flashes, night sweats and mood swings that prevent restful sleep.
- Progesterone: Another hormone that regulates the menstrual cycle, progesterone has a naturally calming and sedative effect. Its levels often fall before menstruation and during menopause, leading to the notion that hormone imbalance can cause insomnia.
- Testosterone: There’s a close connection between testosterone levels and sleep quality. In men, testosterone levels naturally rise during sleep and peak in the morning. Poor or not enough sleep can cause testosterone production to drop, negatively affecting energy, mood and sleep. Low testosterone has also been linked to insomnia.
Common Hormone-Related Sleep Issues
Hormonal imbalances of cortisol, estrogen and progesterone can lead to any of the following sleep issues:
Night Sweats and Hot Flashes
Age-related hormone sleep changes can occur as you enter perimenopause, the years leading up to menopause. Hormones like estrogen and progesterone start declining at this time, which can cause hot flashes and night sweats.
Melatonin levels can also drop, affecting your body’s internal clock. Furthermore, the decline of estrogen can also affect cortisol levels at this life stage, increasing anxiety and making it harder to fall and stay asleep. In fact, insomnia is one of the most common symptoms of menopause, with sleep disturbances in women rising from 16% to 60% at the time of perimenopause through postmenopause.
Fatigue and Muscle Tremors
Research suggests that an imbalance of thyroid hormones can disrupt the circadian rhythm. More specifically, hypothyroidism, or an underactive thyroid, and hyperthyroidism, an overactive thyroid, are conditions that can lead to sleep-related challenges like:
- Anxiety
- Mood shifts and changes
- Fatigue
- Muscle tremors
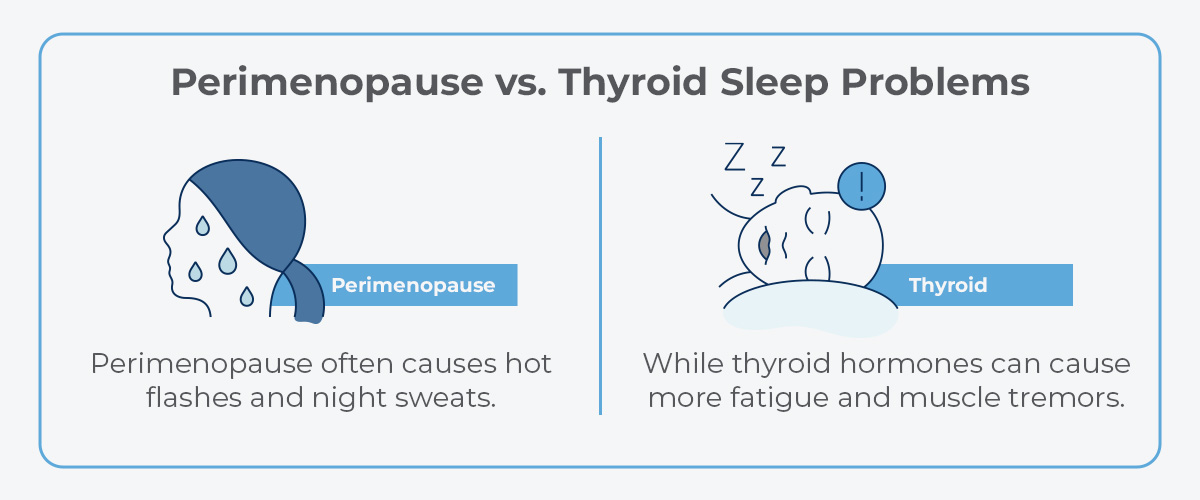
When it comes to perimenopause vs. thyroid sleep problems, perimenopause often causes hot flashes and night sweats, while thyroid hormones can cause more fatigue and muscle tremors.
Stress and Mood Changes
When you experience long-term stress, it also affects hormones throughout your body, like adrenaline and cortisol. These hormonal fluctuations can increase anxiety and make it harder to get a good night’s rest. They can also lead to complications like:
- Depression
- Muscle tension and pain
- Low sex drive
- Heart disease
- Weight gain
Over time, you can experience a stress hormone insomnia cycle, where higher cortisol can lead to insomnia, and poor sleep can increase stress.
Signs Your Sleep Issues May Be Hormone-Related
Certain symptoms can indicate that your sleep issues are related to hormonal changes, like daytime fatigue and waking too early in the morning. Further, the timing of these symptoms can determine whether they are related to hormones. It’s important to look out for the patterns and seek professional help as soon as you notice them. Hormone imbalance sleep symptoms can include:
- Trouble maintaining a sleep schedule
- Daytime fatigue
- Changes in mood
- Irritability or trouble concentrating during the day
- Frequently waking up in the middle of the night and being unable to fall back asleep
- Waking up earlier in the morning than planned
- Difficulty falling asleep after going to bed
If you notice these symptoms in the week before your menstrual cycle, it could indicate that progesterone levels are affecting your sleep, making it harder to fall asleep or get good quality rest. Perimenopause, which often starts in the mid-40s and menopause, which may start in the 50s, can cause nighttime awakenings from hot flashes or night sweats.
Lastly, women who have just given birth can experience a sharp decline in progesterone, leading to mood swings, fatigue and sleep disruptions.
Solutions for Hormone-Related Sleep Problems
Health care professionals might recommend any of the following treatments for hormonal insomnia:
Proper Sleep Hygiene
Proper sleep hygiene is about maintaining a regular sleep schedule, and you can do this in several ways. For example, morning bright light might help suppress lingering melatonin and anchor your circadian rhythm. Dim lights and screens a few hours before bed to allow melatonin to rise naturally. Try to go to bed around the same time every night and wake up at the same time.
Regular Exercise
Regular movement can help regulate hormones related to the sleep-wake cycle. Exercise can also reduce stress-related cortisol and release hormones like endorphins, serotonin and dopamine to promote greater calm — all helpful for a restful night’s sleep.
Healthy Diet
Prioritize balanced meals with protein, fiber and healthy fats to help balance cortisol, insulin, leptin and ghrelin. Consider a protein-rich breakfast and complex carbs at dinner. Use small, easy-to-digest snacks if needed, and avoid caffeine late in the day and alcohol near bedtime, which affect your sleep-wake cycle.
Environmental Changes
You can also make environmental changes conducive to better sleep, such as making your bed comfier with cozy pillows, using blackout curtains to keep out the light or listening to a white noise machine to drown out sounds. A cooler bedroom might also help reduce hot flashes so you can enjoy more restful sleep.
Natural Support Options
Some supplements, like melatonin, might help you fall asleep more easily. Magnesium, glycine and L-theanine might also support relaxation. Contact a health care provider to discuss supplements that are safe for you and ensure the right dosage.
Cognitive behavioral therapy for insomnia (CBT-I) can also treat sleep issues. It involves breathing exercises, mindfulness and other techniques that may help manage stress and relax around bedtime.
Hormone Replacement Therapy
If lifestyle changes aren’t working, your provider might recommend hormone testing for sleep disorders. They can determine if a hormonal imbalance is the reason for your insomnia and advise you on treatment to restore levels to a more balanced state.
Based on results and goals, individualized treatment — such as bioidentical hormone therapy for menopausal symptoms or low testosterone — may be considered after reviewing risks and benefits.
Restore Restful Sleep by Addressing the Hormone Root Cause
Recognizing symptoms of hormonal imbalance is the first step toward restoring restful sleep. At Spartan Medical Associates, we can support your journey with evidence-based, comprehensive treatment plans. Our experienced providers look beyond singular symptoms, addressing your entire health and offering hormone replacement therapy, longevity, biomarker optimization and weight loss solutions.
We deliver our concierge-style approach through telehealth in North Carolina and Delaware. Call 704-237-6512 to request a free phone consultation and start your journey toward better health and restful sleep.